PATIENT: Poppy, 1yr 7m FE Labradoodle
Poppy was referred for further investigations into her cough of >3 weeks duration. Poppy was initially treated symptomatically for suspected kennel cough with NSAIDs and antibiotics, however 1 week into treatment her condition deteriorated.
Thoracic radiographs taken by Poppy’s primary care vets were suggestive of a diffuse bronchopneumonia, at which point a second antimicrobial and furosemide therapy were added to her treatment plan. Poppy continued to deteriorate with periods of cyanosis and dramatic weight loss noted by her owner, so referral was sought.
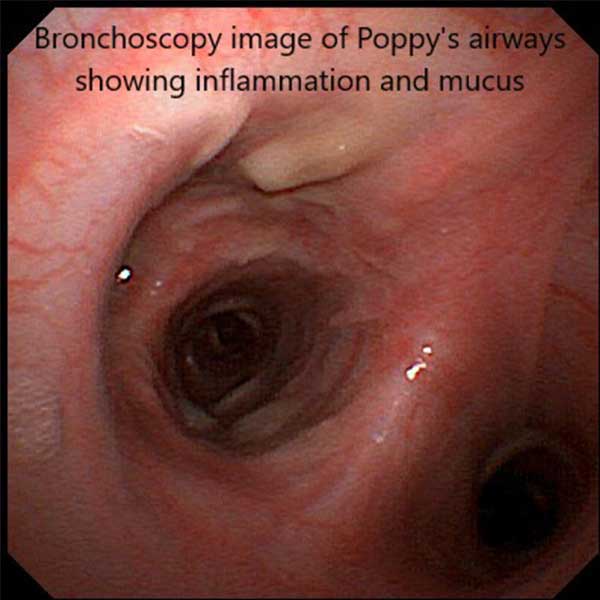
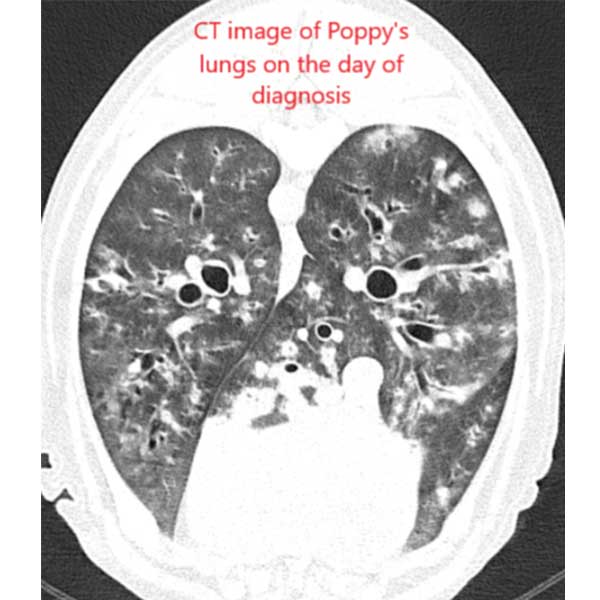
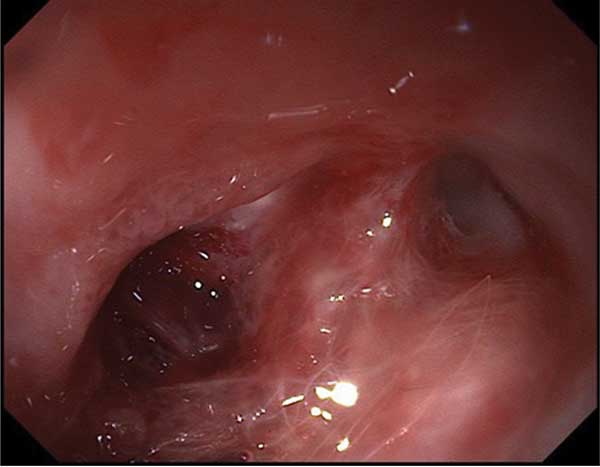
On presentation Poppy was bright, alert and responsive. Diffuse crackles and wheezes were audible throughout her lung fields. Heart rate and rhythm were within normal limits and peripheral pulse quality was good. Poppy was anaesthetised and a CT scan of her thorax carried out which confirmed a very severe, diffuse bronchial pattern with generalised bronchial wall thickening. Several solid, small lung nodules were also noted alongside significant enlargement of the tracheobronchial lymph nodes. Bronchoscopy and BAL sampling was performed. Thick yellow/brown/green discharge was present in both Poppy’s large and small airways. Microscopy of these samples highlighted a marked predominance of eosinophils with occasional neutrophils. No bacteria were seen.
These findings were consistent with a diagnosis of eosinophilic bronchopneumopathy (pulmonary infiltrate with eosinophils or PIE). An Angio-detect lung worm test was found to be negative and there was no evidence to support lungworm infestation in the BAL sampling. 1mg/kg prednisolone once daily was initiated, to which Poppy showed a very good and rapid response.
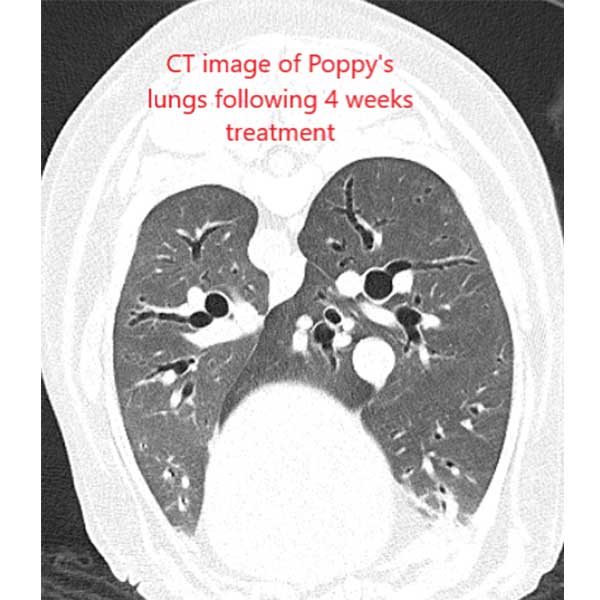
Eosinophilic pulmonary diseases in dogs can be of varying severity, which in turn can affect their response to treatment. We were concerned that the presence of pulmonary nodules and enlarged tracheobronchial lymph nodes in Poppy’s case was indicative of more severe disease, however, she showed a fantastic response to treatment with rapid complete resolution of her clinical signs. A repeat CT scan 4 weeks following initiation of treatment showed a much-improved bronchopneumonia and lymphadenopathy. A mild residual bronchointerstitial, nodular pattern remained – most likely due to a combination of remaining disease and scar type lesions.
Poppy’s prednisolone dose was gradually tapered by 25% every 3-4 weeks with no relapse in clinical signs seen and she remains clinically well now that she is off treatment altogether.