PATIENT: Macintosh 2-year-old male, neutered Ragdoll.
Macintosh, was presented by his breeder as a second opinion
and for further investigations into his recently diagnosed
gastric mass and local lymphadenopathy. Fine needle
aspirates had failed to yield a diagnosis as to the cause, but
a gastric adenoma and reactive lymphadenopathy were
suspected. Further investigations with endoscopy or surgical
biopsies had been offered but declined with his owner
considering euthanasia if his clinical signs could not be
controlled. Palliative care with mirtazipine, maropitant and
weekly dexamethasone injections had been instituted.
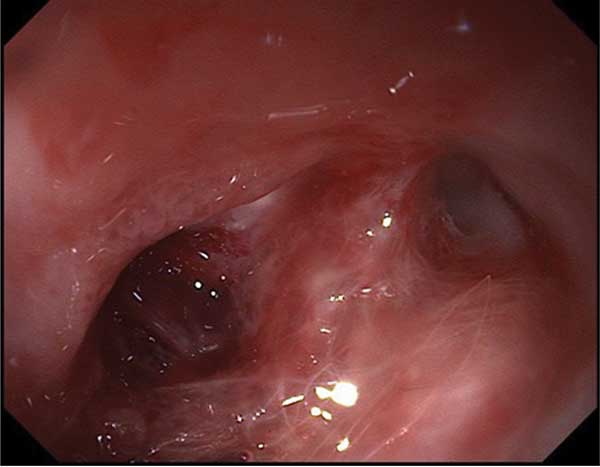
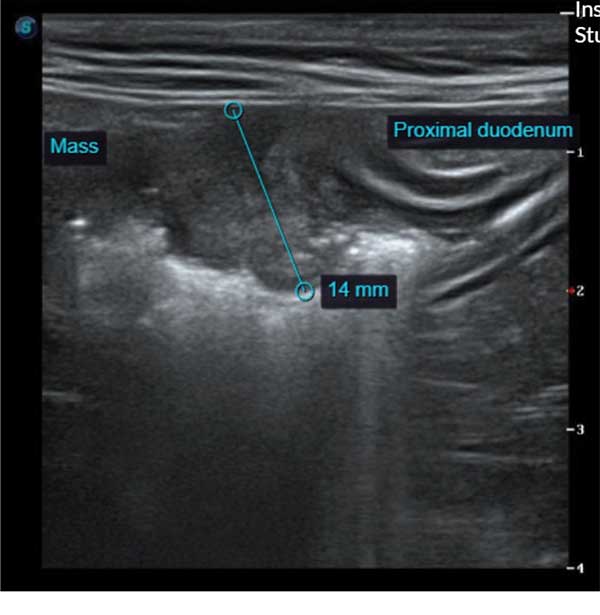
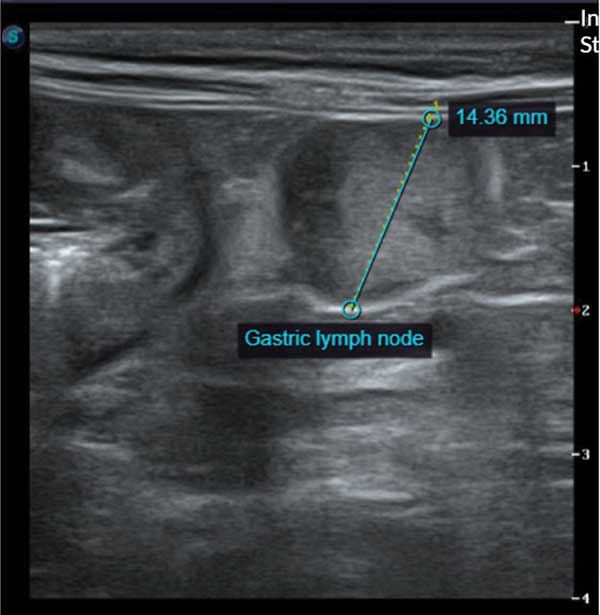
On presentation to Eden Vets Macintosh was bright, alert and responsive. His body condition was good and physical examination was unremarkable. On abdominal ultrasonography the mass could be clearly identified at the junction between the stomach and duodenum with severe wall thickening and loss of layering. The adjacent lymph node was markedly enlarged at 1.5cms diameter. Fine needle aspirates were taken from the lymph node and upper gastrointestinal endoscopy was performed to visualise and biopsy the mass. The mass was located just behind the cardiac sphincter in the very proximal duodenum and was circumferential and ulcerated with an impacted hair ball in the region. The hair ball was dislodged, and multiple biopsies were taken. The remainder of the stomach appeared grossly normal and the duodenum distal to the mass also appeared normal.
Cytology of the lymph node showed mixed population of inflammatory cells (small lymphocytes, some neutrophils, some eosinophils, and rare mast cells). Histopathological examination of the mass was consistent with a very rare condition called feline gastrointestinal eosinophilic sclerosing fibroplasia (FEGSF). This condition is inflammatory in nature with the underlying aetiology unclear. It presents as mass lesions usually near the pylorus or ileocaecocolic junction, with Ragdolls overrepresented in the literature. Optimal treatment is not well established but recommendations have been suggested. Surgical excision with follow-up medical management is recommended, but the location in Macintosh sadly prohibited simple surgical excision as the mass almost certainly involved the biliary and pancreatic ducts. Surgical options do exist in this location, but they are often not recommended as they are very complex and complication rates are high. CT imaging was offered to clarify the exact extent, location, and involvement of the ducts, but was declined by Macintosh’s owner.
Without surgical excision, treatment of FGESF is aimed at controlling ongoing inflammation to try and halt any further growth. A reduction in size of the mass is considered unlikely due to the degree of fibrosis. The current recommendation for this is a combination of prednisolone and cyclosporine. Prednisolone is the mainstay of most inflammatory bowel disorders, but cyclosporine is also recommended because in dogs with eosinophilic IBD it is considered the most effective drug. It is hypothesised that as FGESF is also eosinophilic the same may apply; sadly, however, evidence is currently lacking. Antibiotic therapy is also recommended but an underlying bacterial aetiology has not been proven1.
Macintosh was started on oral prednisolone 1mg/kg PO SID alongside omeprazole 1mg/kg PO SID due to visible ulceration of the mass. Cyclosporine and antibiotic therapy were discussed with Macintosh’s owner but declined. 1 month following diagnosis Macintosh remained well with good control of his clinical signs. 3 months later Macintosh continued to do well however the case was lost to long term follow up thereafter.
Reference:
1. Linton M, Nimmo JS, Norris JM, Churcher R, Haynes S, Zoltowska A, Hughes S, Lessels NS, Wright M, Malik R. Feline gastrointestinal eosinophilic sclerosing fibroplasia: 13 cases and review of an emerging clinical entity. J Feline Med Surg. 2015 May;17(5):392-404. doi: 10.1177/1098612X14568170. PMID: 25896239.