Noah, 6years 4 months, MN, Border collie.
Noah was referred to Eden Vets after being diagnosed with bilateral perineal hernias, complicated by ventral bladder retroflexion into the left hernial sac.
The patient had a prolonged, 18-month history of constipation and tenesmus with a soft reducible perineal swelling first arising from the right side but becoming bilateral over time. He had been managed
medically with stool softeners and periodic digital evacuation. Castration was performed after diagnosis of the primary right sided perineal hernia 12 months previously. Preceding referral the patient presented with clinical signs associated with a urinary obstruction; 24-hour history of stranguria and lethargy alongside a firm and turgid left sided perineal swelling. Definitive diagnosis of bladder involvement was accomplished by centesis of urine from the perineal mass at the primary care vets.
Digital rectal examination revealed loss of the normal pelvic diaphragm with the presence of a presence of a fluctuant mass (bladder) in the left perineum and pelvic viscera within the right hernial sac. Haematology
and biochemistry panels demonstrated a mild-moderate inflammatory leucogram with no sign of an azotaemia or electrolytes disturbances. Urinalysis revealed haematuria (in absence of infection) presumed
consequence of bladder trauma during retroflexion.
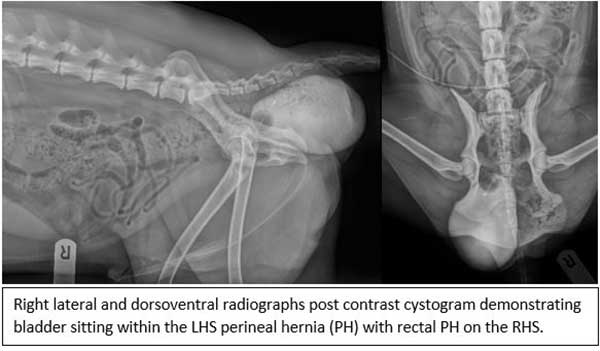
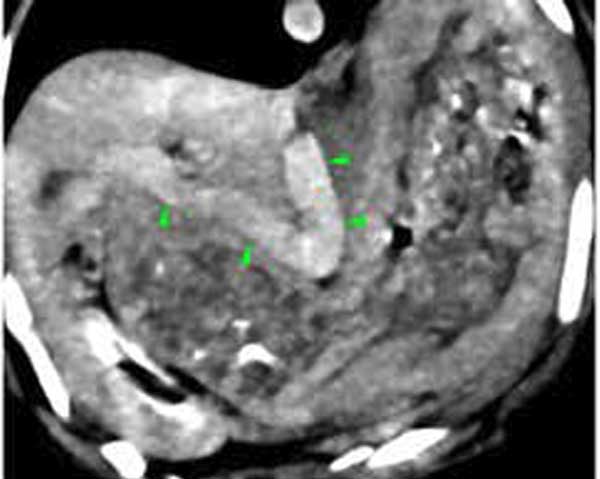
Abdominal ultrasonography and retrograde contrast cystogram were performed to identity bladder position and to rule out the presence of a uroperitoneum. Thankfully no urinary tract rupture had occurred.
Prostatomegaly (presumed benign prostatic hyperplasia) was the only other significant finding upon ultrasound. An 8F indwelling urinary catheter and sterile collection device was used to allow for supportive
care prior to surgical intervention.
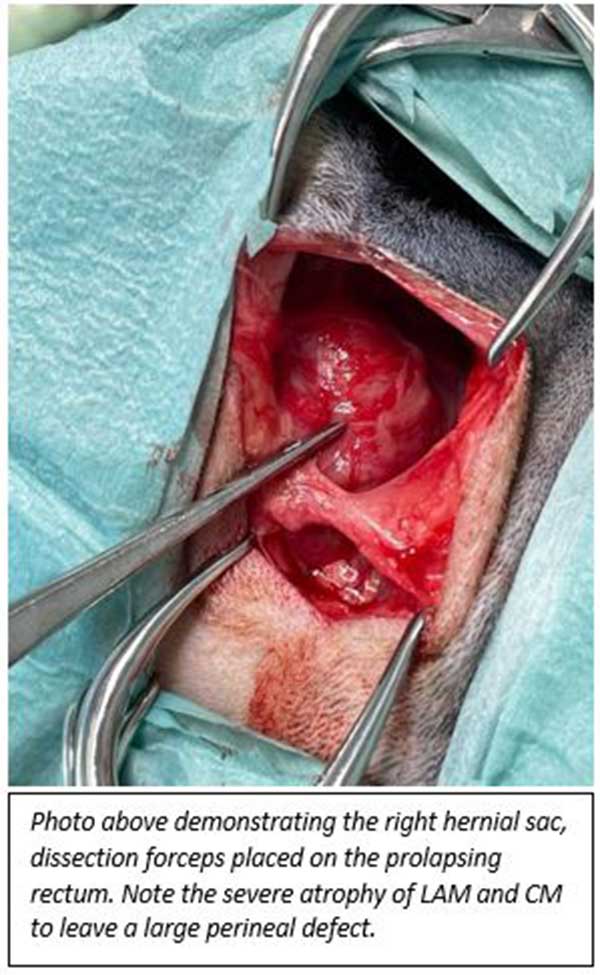
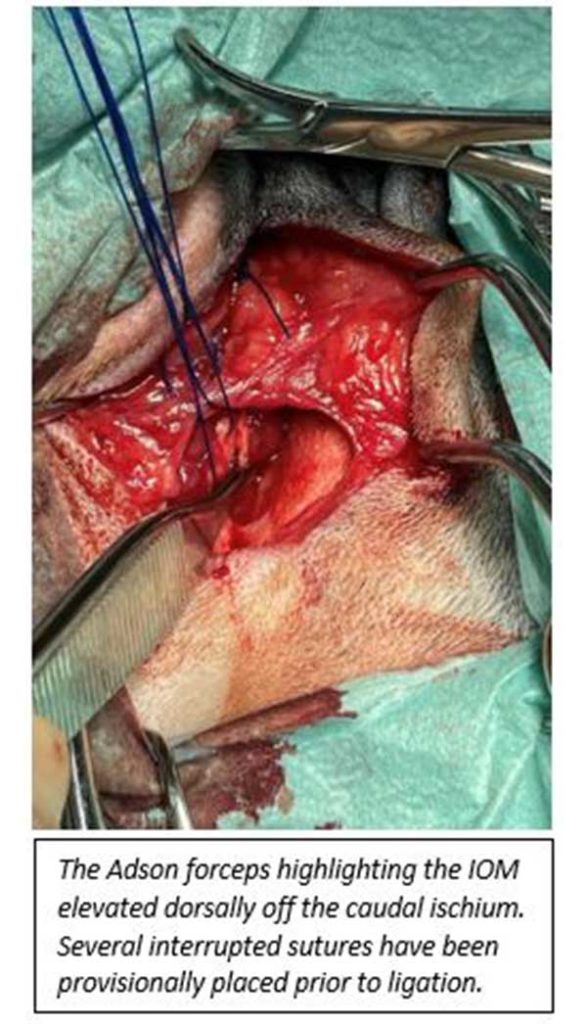
Surgical management of perineal hernia typically involves reconstruction of the pelvic diaphragm by anatomic muscle apposition of transposition of regional muscle flaps. In this case an internal obturator (IOM) flap was elevated dorsally from the ischium bilaterally. The defects were closed using several preplaced, interrupted sutures of 3.5M Prolene beginning dorsally between the external anal sphincter (EAS) and Coccygeus muscles (CM), continuing ventrally to include suturing around the Sacrotuberous ligament to IOM, EAS and CM. Excellent closure of the hernia site was achieved bilaterally. Cystopexy via ventral midline celiotomy was performed as an adjunct to herniorrhaphy to prevent repeated bladder retroflexion and subsequent complications.
Noah remained hospitalised for several days prior to being discharged. Overall, he recovered well from the procedure however did suffer from excessive straining presumably due to postsurgical pain in the
immediate post operative period. This settled over the subsequent weeks and since has been reportedly doing well with no tenesmus, reoccurrence of the hernias nor urinary tract signs.